Sexual Health
Study Shows HPV Vaccine Doesn’t Lead To Promiscuity
The Human Papillomavirus (HPV) is a common sexually transmitted infection that most of us will encounter over our lifespans. Most people will never show symptoms. Women with HPV may have nothing more than an abnormal pap smear that resolves within a year or two. There are over 100 strains of HPV, about 40 of which affect the mouth and genitals. While most of these are harmless, there are high risk strains such as HPV 16 and HPV 18 can cause serious health issues such as rectal, cervical, penile, and throat cancer. Additionally, low risk strains like HPV 6 and HPV 11 can cause genital warts to develop. The strains that cause cancer do not cause warts, and vice versa. While using condoms can help reduce the risk of transmitting HPV to some degree, there is no form of contraception that is 100% effective against HPV.
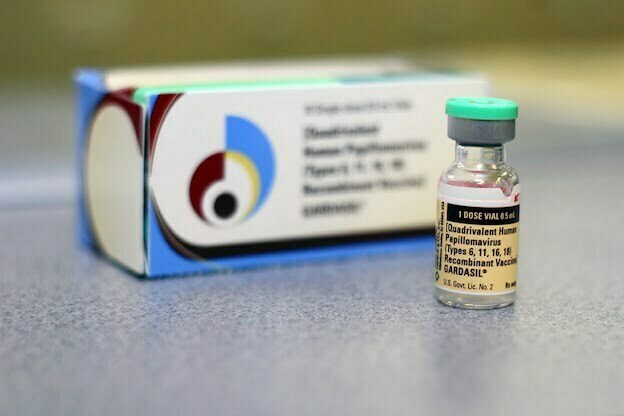
Fortunately, HPV vaccinations such as Gardasil and Cervarix, can prevent these aggressive strains and are recommended for adolescents of all genders before they become sexually active. Gardasil protects against the two types of HPV that cause 75% of cervical cancer cases, and the two types that cause 90% of genital wart cases. Cervarix only offers protection against the cancer causing strains. Vaccination is suggested between the ages of 11 and 12, but can be administered to individuals up to age 26.
Vaccination panic
In spite of its success as the only known vaccine to prevent any type of cancer, the HPV vaccination is running into some PR issues. A small faction of parents claim that the vaccination can be lethal or lead to autism, although these claims are highly contested. What seems to be a larger barrier for vaccination efforts is the belief that being vaccinated will encourage risky sexual behavior. Parents and even some clinicians are concerned that this added protection against STIs might lead teens to engage in riskier and more frequent sexual behaviors.
HPV vaccine doesn’t influence sexual behavior
In a 2014 study published in the Journal for Pediatric and Adolescent Gynecology, researchers put this belief to the test. Rysavy et al. compared the self-reported sexual behavior of 153 vaccinated and 70 unvaccinated young women (n=223) to investigate if receiving the HPV vaccination would contribute to high-risk sexual acts. The average age of the unvaccinated and vaccinated samples were 20.1 and 19.2 years old, respectively.
After querying participants about previous sexual experience and number of partners, the authors found no significant difference between the vaccinated and unvaccinated young women. In fact, Rysavy et al. indicated that both groups were engaging in high-risk sexual behaviors; only 20-25% of the participants reported using condoms in all sexual encounters. The age at which respondents first engaged in various sexual behaviors proved to be similar across groups as well. This finding indicates that the HPV vaccination does not lead adolescents to engage in risky sexual behavior; rather, it is this misconception that actually puts unvaccinated teens at a greater risk for health concerns.
Ultimately, the authors conclude, the riskiest behavior is preventing adolescents from acquiring the HPV vaccination.
Interested in Being Vaccinated?
Previously, some insurance companies did not cover the round of vaccinations against HPV, and many people find the series too expensive to pay for independently. As a result of the new health care reform, most people will be able to receive coverage for Gardasil and Cervarix. There are also several sources of public financing available for the HPV vaccination, depending on demographics and location. Merck, the developer of Gardasil, also offers a patient assistance program that can cover the cost of the shots.